Interstitial ectopic pregnancy is a rare but serious type of ectopic pregnancy that accounts for only 2–4% of all cases. Unlike tubal ectopics that present early, interstitial pregnancies often appear later—between 7 to 12 weeks of gestation—making them difficult to detect and potentially life-threatening if missed.
This blog explains the causes, risk factors, symptoms, diagnosis, and treatment options for interstitial ectopic pregnancy, along with a real-life case to highlight its importance.
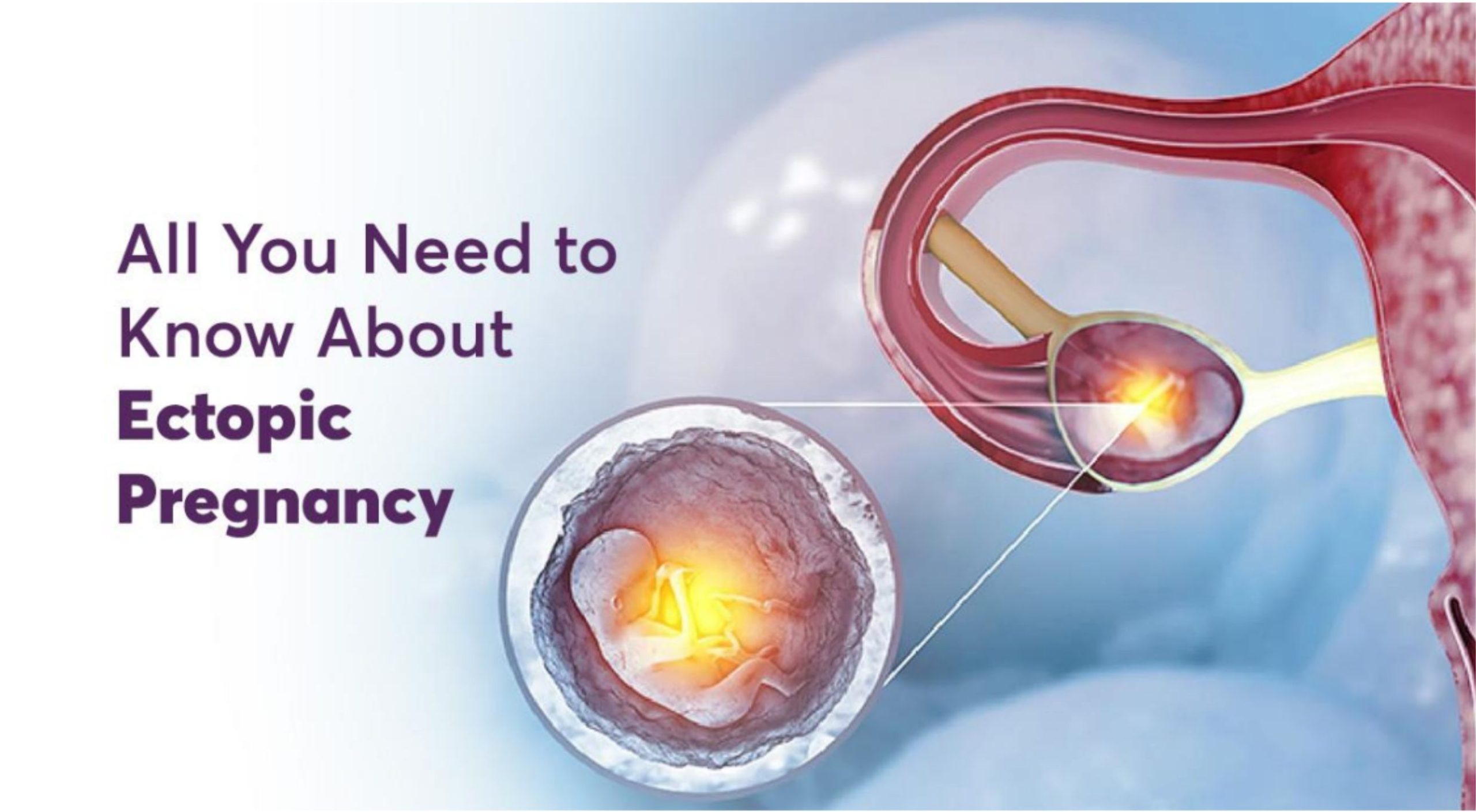
What is an Interstitial Ectopic Pregnancy?
An ectopic pregnancy occurs when a fertilized egg implants outside the uterine cavity. In an interstitial ectopic pregnancy, the embryo implants in the interstitial portion of the fallopian tube, the section that passes through the muscular wall of the uterus.
Because this part of the uterus can stretch, the pregnancy may grow larger before rupturing. However, when rupture occurs, the risk of internal bleeding and shock is far greater compared to other ectopic pregnancies, making it a medical emergency.
Risk Factors for Interstitial Ectopic Pregnancy
Women may be at a higher risk if they have:
- History of pelvic inflammatory disease (PID)
- Previous ectopic pregnancy
- Pelvic or tubal surgery
- Use of assisted reproductive technologies (ART/IVF)
- Advanced maternal age
- Smoking
- Congenital uterine anomalies
Warning Signs and Symptoms
The challenge with interstitial ectopic pregnancy is that symptoms can resemble normal pregnancy or other abdominal conditions.
Common warning signs include:
- Severe abdominal or pelvic pain
- Intermittent vaginal bleeding
- Nausea and vomiting due to pregnancy hormones
- Dizziness, fainting, or low blood pressure (signs of internal bleeding)
If you notice these symptoms in early pregnancy, seek medical attention immediately.
How is Interstitial Ectopic Pregnancy Diagnosed?
Early diagnosis is crucial to prevent complications. Doctors rely on:
- Ultrasound (USG) of the pelvis to detect abnormal implantation
- Serial serum Beta-hCG levels to check abnormal hormone rise patterns
Treatment & Management Options
The management of interstitial ectopic pregnancy depends on the patient’s condition, pregnancy stage, and fertility considerations.
1. Surgical Management
- Laparoscopic surgery is the standard treatment.
- Options include wedge resection (removing the ectopic tissue while preserving the uterus) or removal of the affected tube.
2. Medical Management
- In selected stable cases, Methotrexate injection may be used to stop the pregnancy tissue from growing.
Case Report: Early Detection Saved a Life
We recently treated a 37-year-old pregnant woman who presented with abdominal pain. Her pregnancy test was positive, and beta-hCG levels corresponded to 9 weeks of gestation.
An ultrasound confirmed an interstitial ectopic pregnancy. She underwent laparoscopic wedge resection with removal of the affected tube. Remarkably, she was discharged within 24 hours.
This case highlights the life-saving importance of early diagnosis. Without timely surgery, risks included:
- Severe hemorrhage
- Hypotensive shock
- Emergency hysterectomy (removal of the uterus)
Conclusion: Awareness is the Key
Though rare, interstitial ectopic pregnancy is dangerous if missed. Early recognition, timely diagnosis, and appropriate treatment can reduce complications and preserve fertility.
Women should be educated about early pregnancy symptoms and encouraged to seek prenatal care immediately after a missed period.
Dr. Rajani Vaidya
MBBS, MS OBG, FMAS Fellowship in Minimal Access Surgery, FALS ROBOTICS
Consultant – Obstetrics and Gynecology Minimally Invasive and Robotic Gynecologic Surgery.