Overview
Bladder cancer forms in the lining of the bladder, the organ that stores urine. It is more common in men than in women and usually appears after the age of 55.
Main Types
- Urothelial (transitional cell) carcinoma – ~90 % of cases; arises from the inner lining.
- Squamous cell carcinoma – linked to chronic irritation (e.g., long‑term catheter use, bladder stones).
- Adenocarcinoma – rare; associated with long‑standing inflammation.
Risk Factors (India & globally)
- Smoking (responsible for ~50 % of cases)
- Occupational exposure to aromatic amines (dyes, rubber, textiles)
- Chronic bladder irritation (infection, stones, catheter)
- Previous pelvic radiation or certain chemotherapy drugs
- Family history or genetic predisposition
Common Symptoms
- Blood in urine (hematuria) – often painless – Frequent or urgent urination
- Dysuria (burning sensation)
- Pelvic or lower back pain (advanced disease)
How It’s Diagnosed
- Urine tests – cytology, urine markers
- Cystoscopy – direct visual inspection of the bladder
- Imaging – ultrasound, CT urography, MRI
- Biopsy – tissue taken during cystoscopy for definitive diagnosis
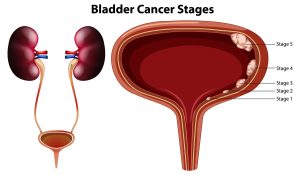
- Staging – CT/MRI of abdomen‑pelvis, chest imaging, bone scan if needed
Treatment Options (stage‑dependent)
- Non‑muscle‑invasive (early) disease
- Transurethral resection of bladder tumor (TURBT) + intravesical therapy (BCG vaccine or chemotherapy)
- Surveillance cystoscopy every 3‑6 months
- Muscle‑invasive disease
- Radical cystectomy (removal of bladder, prostate in men; uterus and anterior vagina in women) with urinary diversion (ileal conduit, neobladder, continent pouch)
- Neoadjuvant chemotherapy followed by surgery
- Bladder‑preserving trimodal therapy (maximal TURBT + chemoradiation) for selected patients
- Metastatic disease
- Systemic chemotherapy (gemcitabine + cisplatin or dose‑dense MVAC)
- Immunotherapy (pembrolizumab, atezolizumab) for advanced or cisplatin‑ineligible cases
- Targeted agents in clinical trials (e.g., FGFR inhibitors)
Prognosis
- 5‑year survival > 90 % for non‑muscle‑invasive tumors that are completely resected.
- Drops to 50‑70 % for muscle‑invasive disease treated with surgery ± chemotherapy.
- Metastatic disease has a poorer outlook, but immunotherapy has improved survival in recent years.
Follow‑up
- Regular cystoscopy and urine cytology for at least 5 years after treatment.
- Imaging (CT/MRI) as guided by risk factors.
Prevention Tips
- Quit smoking – the single most effective measure.
- Maintain a healthy weight and stay hydrated.
- Use protective equipment if you work with industrial chemicals.
- Promptly treat urinary infections or stones to reduce chronic irritation.
If you have specific concerns—such as symptoms you’re experiencing, questions about a recent diagnosis, or need help finding a urologist in India—let me know and I can provide more targeted information.
Dr. V. Manjunath
MBBS, MS (General Surgery), MCh (Urology)
Consultant – Urology & Andrology